Fungi as a pathogen
Table of content
- Definition
- Introduction to Fungi as a Pathogen
- Systemic Mycoses and Primary Site of Infection
- Factors Contributing to Infection and Pathogenesis of Fungi
- Role of Morphologic Transformation in Fungal Infection
- Hostile Cellular Environment of the Lungs
- Capsular Polysaccharide as a Determinant of Virulence
- Elaboration of Phenyl Oxidase and Virulence
- Mechanisms of Fungal Pathogenicity
- Conclusion
Definition
Fungi are organisms that can cause disease in plants, animals, and humans. When a fungus invades a living host, it can grow and reproduce, leading to a range of health problems. Fungal infections can occur in different parts of the body, such as the skin, nails, lungs, and bloodstream, and can be mild or severe, depending on the type of fungus and the individual's immune system.
Some common examples of fungal pathogens include Candida, Aspergillus, and Cryptococcus, which can cause infections such as thrush, aspergillosis, and cryptococcosis, respectively.
Introduction
Fungi are ubiquitous in nature and can be found in various environments such as soil, water, and air. While many fungi are harmless, some have the ability to cause infection and disease in humans and other animals. Fungal infections, also known as mycoses, can range from mild skin infections to severe systemic infections that can be life-threatening.
we will discuss the various factors that contribute to the pathogenesis of fungi, including their ability to adapt to the host environment, their morphological changes, and the virulence factors they produce. We will also highlight the importance of studying fungal pathogenesis, particularly in light of the increasing incidence of opportunistic infections.
Fungi rarely cause disease in healthy immunocompetent hosts. Disease results when fungi accidentally penetrate host barriers or when immunologic defects or other debilitating conditions exist that favor fungal entry and growth.
Before a specific fungus can be confirmed as the cause of a disease, the same fungus must be isolated from serial specimens, and fungal elements morphologically consistent with the isolate must be observed in tissues taken from the lesion. In general, fungal infections and the diseases they cause are accidental. A few fungi have developed a commensal relationship with humans and are part of the indigenous microbial flora (e.g., various species of Candida, especially Candida albicans, and Malassezia furfur).
Although a great deal of information is available concerning the molecular basis of bacterial pathogenesis, little is known about the mechanisms of fungal pathogenesis. Infection is defined as entry into body tissues followed by multiplication of the organism. The infection may be clinically inapparent or may result in disease due to a cellular injury from competitive metabolism, elaboration of toxic metabolites, replication of the fungus, or an immune response.
Immune responses may be transient or prolonged and may be cell-mediated, humoral (with the production of specific antibodies to components of the infecting organism), or both. Successful infection may result in disease, defined as a deviation from or interruption of the normal structure or function of body parts, organs, or systems (or combinations thereof) that is marked by a characteristic set of symptoms and signs and whose etiology, pathology, and prognosis are known or unknown.
Systemic Mycoses and Primary Site of Infection
Systemic mycoses are fungal infections that affect various organs and tissues throughout the body, including the lungs, brain, and skin. These infections occur when fungi, such as Aspergillus, Candida, and Cryptococcus, enter the body and begin to grow and spread.
The primary site of infection for systemic mycoses varies depending on the type of fungus. For example:
Aspergillosis:
Aspergillosis is caused by Aspergillus fungi and can affect the lungs, sinuses, and other organs. In some cases, the infection can spread to other parts of the body, such as the brain or heart.
Candidiasis:
Candidiasis is caused by Candida fungi and can affect various parts of the body, including the mouth, throat, and genitals. In severe cases, the infection can spread to the bloodstream and other organs.
Cryptococcosis:
Cryptococcosis is caused by Cryptococcus fungi and can affect the lungs, brain, and other organs. The infection is typically acquired by inhaling fungal spores from the environment.
Other types of systemic mycoses include histoplasmosis, blastomycosis, and coccidioidomycosis, which are caused by Histoplasma, Blastomyces, and Coccidioides fungi, respectively. These infections can also affect various organs and tissues in the body.
Systemic mycoses can be difficult to diagnose and treat, and they can be life-threatening in some cases. Treatment typically involves antifungal medications, and in some cases, surgery may be necessary to remove infected tissue. It is important to seek medical attention if you suspect you may have a fungal infection.
Factors Contributing to Infection and Pathogenesis of Fungi
Fungal infections can occur in individuals with weakened immune systems or those with a predisposition to fungal infections. Several factors can contribute to the development of fungal infections and their pathogenesis.
Immune System:
A weakened immune system is the most common factor contributing to fungal infections. This includes individuals with HIV/AIDS, cancer patients undergoing chemotherapy, and individuals on long-term corticosteroid therapy.
Environmental Factors:
Environmental factors such as humidity, temperature, and exposure to fungal spores can contribute to the development of fungal infections. Fungi thrive in warm and moist environments and can infect individuals through inhalation or skin contact.
Genetics:
Genetic factors can also contribute to the development of fungal infections. Certain genetic disorders such as chronic granulomatous disease (CGD) can make individuals more susceptible to fungal infections.
Lifestyle Factors:
Certain lifestyle factors such as poor nutrition, smoking, and alcohol consumption can also increase the risk of fungal infections.
Microbial Interactions:
Fungal infections can also occur due to microbial interactions. For example, fungal infections can develop in individuals who have been treated with broad-spectrum antibiotics that kill off beneficial bacteria, allowing fungi to proliferate.
Pathogenesis of fungal infections involves several stages, including adhesion to host cells, invasion of host tissues, and colonization. Once the fungi have colonized the host, they can cause tissue damage through various mechanisms such as the production of toxins, invasion of host cells, and induction of an inflammatory response.
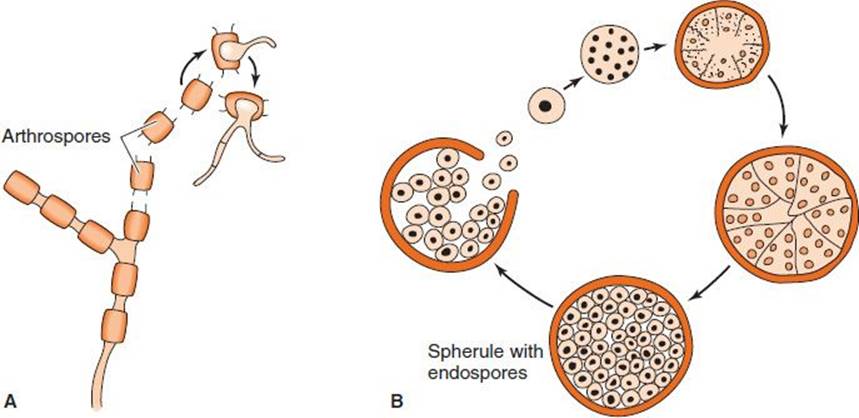
Role of Morphologic Transformation in Fungal Infection
Fungi have the ability to switch between different morphological forms, which can play a critical role in their ability to cause infections. This process is known as morphologic transformation and it occurs in response to environmental cues and host factors.
One example of this is the transformation of the fungus Candida albicans from a harmless, single-celled yeast form to an invasive filamentous form, which can cause serious infections in immunocompromised individuals. The transition to the filamentous form is thought to be triggered by the host immune system, as well as factors such as pH, temperature, and nutrient availability.
Another example is dimorphic fungi, which can switch between a yeast form and a filamentous form depending on the environmental conditions. For example, the fungus Histoplasma capsulatum exists in a filamentous form in the soil and a yeast form in the host. The yeast form is better adapted for survival in the host and is responsible for causing disease.
Morphologic transformation can also contribute to antifungal resistance. For example, the fungus Aspergillus fumigatus can switch to a highly resistant, dormant form called a conidium in response to stress, making it more difficult to treat with antifungal medications.
The ability of fungi to undergo morphologic transformation plays a crucial role in their pathogenesis and ability to cause disease. Understanding this process is important for developing new treatments and strategies to prevent and control fungal infections.
Hostile Cellular Environment of the Lungs
The lungs are considered one of the most hostile environments for pathogens due to their complex and sophisticated defense mechanisms. The respiratory tract is lined with specialized cells and molecules that work together to prevent infections. For example, the cilia and mucus in the airways trap and remove foreign particles, while macrophages and other immune cells constantly monitor the lung tissue for any invading pathogens.
However, fungi have evolved several mechanisms to overcome these defense mechanisms and establish an infection. Fungi can produce enzymes that degrade host tissues and help them to invade deeper into the lung tissue. They can also produce toxins that damage or kill host cells, allowing the fungi to colonize and establish themselves.
In addition, some fungi can transform their morphology in response to different environmental conditions. This allows them to adapt and survive in different niches within the host. For example, some fungi can switch from a yeast form to a filamentous form, which allows them to penetrate deeper into the lung tissue.
The hostile cellular environment of the lungs presents a significant challenge for fungal pathogens, but the ability of fungi to adapt and overcome host defenses highlights the importance of continued research into understanding the mechanisms of fungal infection and pathogenesis.
Capsular Polysaccharide as a Determinant of Virulence
Fungal polysaccharides are important virulence factors that contribute to the ability of fungi to cause disease in humans. Capsular polysaccharides, in particular, are known to play a significant role in the virulence of some fungal pathogens. These polysaccharides form a thick layer around the fungal cell wall, which can help the fungus evade host immune responses and establish infection.
Capsular polysaccharides can interfere with the ability of phagocytic cells to recognize and engulf the fungus, making it more difficult for the host to clear the infection. In addition, some capsular polysaccharides have been shown to inhibit the activity of complement, a key component of the innate immune system.
The specific structure of the capsular polysaccharide can also contribute to virulence. For example, the capsular polysaccharide of Cryptococcus neoformans is composed primarily of glucuronoxylomannan (GXM), which is highly immunosuppressive and inhibits the function of macrophages and other immune cells. The capsular polysaccharide of Aspergillus fumigatus is composed primarily of galactomannan, which has been shown to interfere with the function of dendritic cells, another important component of the immune system.
Capsular polysaccharides are important virulence factors that contribute to the ability of fungi to cause disease in humans. Understanding the structure and function of these polysaccharides may provide insights into the development of new antifungal therapies.
Elaboration of Phenyl Oxidase and Virulence
Phenol oxidase is an enzyme that plays an important role in the virulence of certain fungal pathogens. This enzyme is responsible for the oxidation of phenolic compounds, which results in the production of highly reactive quinones that can cause cellular damage.
In some fungi, such as Cryptococcus neoformans, the production of phenol oxidase is regulated by a gene called laccase. This gene is found on the surface of the fungal cell and is responsible for the production of melanin, a pigment that helps protect the fungus from the host immune system.
Studies have shown that phenol oxidase plays a key role in the virulence of C. neoformans. This is because the enzyme is able to generate reactive oxygen species (ROS) that can damage host tissues and impair the function of immune cells.
In addition to its role in virulence, phenol oxidase has also been studied for its potential use in diagnostic tests for fungal infections. For example, the detection of phenol oxidase activity in patient samples can be used as a diagnostic tool for certain fungal infections, such as aspergillosis.
Mechanisms of Fungal Pathogenicity
Fungal pathogenicity involves a complex interplay of factors that facilitate infection and colonization of host tissues. The mechanisms of fungal pathogenicity can be broadly classified into three categories: invasion, immune evasion, and tissue damage.
Invasion:
Fungi use various strategies to invade host tissues. These include the production of hydrolytic enzymes, such as proteases and lipases, which degrade host tissue barriers, allowing fungal penetration. Fungi can also use mechanical pressure to penetrate tissues. In addition, some fungi can produce specialized structures, such as appressoria or haustoria, which facilitate penetration.
Immune Evasion:Fungi can evade host immune responses by several mechanisms. One way is by masking their pathogen-associated molecular patterns (PAMPs) with a glycocalyx or capsule, which makes them less recognizable to host immune cells. Fungi can also alter their cell surface antigens or secrete immunomodulatory molecules that interfere with host immune responses. Furthermore, some fungi can survive within host phagocytes, such as macrophages, by inhibiting phagolysosome fusion or by escaping phagosomes.
Tissue Damage:
Fungal colonization and invasion can lead to tissue damage through several mechanisms. Fungi can secrete toxins or reactive oxygen species that damage host cells. They can also induce host cell apoptosis or necrosis, leading to tissue damage. Fungi can also induce host inflammatory responses, leading to tissue damage through the release of pro-inflammatory cytokines.
Subcutaneous Mycoses
Subcutaneous mycoses are fungal infections that affect the subcutaneous tissue layers. These infections are caused by fungi that are commonly found in the environment and gain access to the tissues through traumatic implantation.
Pathogenesis and Clinical Manifestations
Little is known about the mechanisms of pathogenesis of subcutaneous mycoses. However, histopathological evidence suggests that these fungi survive in the subcutaneous tissues by producing proteolytic enzymes and maintaining a facultative microaerophilic existence. Clinical manifestations of subcutaneous mycoses vary depending on the causative organism.
Mycotic Mycetoma
Mycotic mycetoma is characterized by extensive tissue damage and the production of purulent fluid that exudes through numerous intercommunicating sinus tracts.
Chromoblastomycosis
Chromoblastomycosis is caused by a group of darkly pigmented (dematiaceous) fungi that exhibit pleomorphism consisting of two distinct morphologies: a mycelial state and a thick-walled spherical cell that divides by cleavage. The latter cell morphology, called a muriform cell, sclerotic cell, or Medlar body, is the pathologic morphology seen in tissue sections.
Sporotrichosis
Sporotrichosis is caused by Sporothrix schenckii, which grows as a mold in nature or when cultured at 25°C, but as yeast-like cells when found in tissues. The clinical manifestations of disease caused by S. schenckii vary, depending on the immune status of the patient.
Conclusion
Fungi are important pathogens capable of causing a variety of diseases in humans, ranging from mild skin infections to life-threatening systemic mycoses. The pathogenicity of fungi is a complex process that involves a number of virulence factors and mechanisms.
These include the ability of fungi to adapt to different environmental conditions, their capacity to evade the host immune response, and their ability to adhere to and invade host tissues. In addition, fungal pathogenicity is also influenced by host factors such as immune status, underlying medical conditions, and genetic predisposition. Understanding the mechanisms of fungal pathogenicity is essential for the development of effective diagnostic and therapeutic strategies for fungal infections.
FAQS
How can fungi act as a pathogen?
Fungi can act as a pathogen by infecting plants, animals, and humans. Fungal pathogens cause a wide range of diseases, including superficial infections such as ringworm, as well as more serious infections such as pneumonia and meningitis.
Fungi can infect their host in several ways, including inhalation of spores, ingestion of contaminated food or water, or direct contact with infected tissue. Once inside the host, fungi can cause damage by releasing toxins or by physically invading and destroying host tissue.
Some fungi are more likely to cause disease in individuals with weakened immune systems, such as those with HIV/AIDS or who have undergone chemotherapy. Additionally, certain types of fungi may be more virulent than others and can cause more severe disease.
Treatment for fungal infections typically involves antifungal medications, which can target the specific type of fungus causing the infection. Prevention measures may include avoiding contact with contaminated soil or other sources of fungal spores, practicing good hygiene, and treating underlying medical conditions that may increase the risk of fungal infections.
Are fungi examples of pathogens?
Yes, fungi are examples of pathogens. Fungal pathogens can cause a variety of diseases in plants, animals, and humans. Some well-known examples of fungal pathogens include Candida albicans, which can cause infections in humans such as thrush, and Aspergillus fumigatus, which can cause lung infections in people with weakened immune systems. Other fungal pathogens can cause diseases in crops, such as rusts and smuts in wheat and other grains. Overall, fungi are important and diverse pathogens that can cause a wide range of diseases and have a significant impact on human and animal health, as well as on agriculture and the environment.
What are 4 fungi considered true pathogens?
There are several fungi that are considered true pathogens because they have the ability to cause disease in otherwise healthy individuals. Here are four examples:
Histoplasma capsulatum: This fungus is found in soil contaminated with bird or bat droppings and can cause histoplasmosis, a respiratory infection that can range from mild to severe and can be fatal if left untreated.
Cryptococcus neoformans: This fungus is found in soil contaminated with bird droppings and can cause cryptococcosis, a respiratory and central nervous system infection that can be life-threatening, especially in people with weakened immune systems.
Blastomyces dermatitidis: This fungus is found in soil and can cause blastomycosis, a respiratory and systemic infection that can be severe and even fatal if left untreated.
Coccidioides immitis and Coccidioides posadasii: These fungi are found in soil in arid regions and can cause coccidioidomycosis, a respiratory infection that can range from mild to severe and can spread to other parts of the body, such as the skin and bones.
It's important to note that these are just a few examples of true fungal pathogens, and there are many other fungi that can cause disease in humans and animals.
Why fungi are successful as pathogens?
Fungi are successful as pathogens for several reasons:
Ability to adapt: Fungi are highly adaptable and can survive in a wide range of environments, including inside the host organism. This adaptability allows them to evade the host's immune system and persist in the body, causing chronic infections.
Production of virulence factors: Fungi produce a variety of virulence factors, such as enzymes, toxins, and adhesins, which enable them to invade and colonize host tissues, evade the immune system, and cause damage to host cells and tissues.
Production of spores: Fungi produce spores that can be easily dispersed through the air, water, or soil, allowing them to spread quickly and infect new hosts.
Production of biofilms: Some fungi can form biofilms, which are complex communities of microorganisms that are highly resistant to antibiotics and immune defenses. Biofilms can protect the fungus from host defenses and allow it to persist in the body.
Nutritional versatility: Fungi are highly adaptable to different nutrient sources and can grow on a wide range of substrates. This flexibility allows them to survive in different environments, including inside the host organism, where they can obtain nutrients from host tissues.
Overall, these factors make fungi highly successful as pathogens, and they are responsible for a wide range of diseases in humans, animals, and plants.
What are the steps of fungal pathogenesis?
The steps of fungal pathogenesis can vary depending on the specific fungus and the host organism involved. However, here are some general steps that many fungal pathogens follow:
Adherence: The first step in fungal pathogenesis is the adherence of the fungus to host tissues. This is often facilitated by adhesins on the surface of the fungus that bind to specific receptors on host cells.
Invasion: Once the fungus has adhered to host tissues, it must then invade the host. This is accomplished through various mechanisms, such as the secretion of enzymes that break down host tissue, penetration of host cells, or phagocytosis by host immune cells.
Colonization: After invasion, the fungus must colonize the host tissue to establish an infection. This involves the growth and replication of the fungus within the host tissue.
Evasion of host defenses: To avoid being eliminated by the host's immune system, the fungus must evade or subvert host defenses. This can be accomplished through a variety of mechanisms, such as the production of toxins or enzymes that damage host immune cells, or inhibition of host immune signaling pathways.
Disease manifestation: The final step in fungal pathogenesis is the manifestation of disease symptoms in the host. These symptoms can vary widely depending on the specific fungus and the host tissue involved and may include fever, inflammation, tissue damage, or organ dysfunction.
What are the top 10 fungal pathogens?
The top 10 fungal pathogens can vary depending on geographic region, host species, and other factors. However, here is a list of 10 fungal pathogens that are commonly associated with human disease:
Candida albicans:
This fungus is a common cause of superficial and systemic infections, particularly in people with weakened immune systems.
Aspergillus fumigatus:
This fungus is a leading cause of invasive aspergillosis, a serious and often fatal infection that primarily affects people with weakened immune systems.
Cryptococcus neoformans:
This fungus is a leading cause of meningitis, particularly in people with weakened immune systems.
Histoplasma capsulatum:
This fungus is a common cause of histoplasmosis, a respiratory infection that can range from mild to severe and can be fatal in people with weakened immune systems.
Coccidioides immitis and Coccidioides posadasii:
These fungi are common causes of coccidioidomycosis, a respiratory infection that can be severe and can spread to other parts of the body.
Pneumocystis jirovecii:
This fungus is a leading cause of pneumonia in people with weakened immune systems, particularly those with HIV/AIDS.
Fusarium spp:
These fungi can cause a wide range of infections in humans, including skin infections, eye infections, and invasive infections in people with weakened immune systems.
Mucorales:
This group of fungi can cause a wide range of infections, particularly in people with diabetes or other underlying medical conditions.
Sporothrix schenckii:
This fungus can cause a skin infection known as sporotrichosis, which is often associated with gardening or other activities that involve contact with soil.
Paracoccidioides brasiliensis:
This fungus is a common cause of paracoccidioidomycosis, a respiratory infection that primarily affects people in Latin America.
What is the classification of fungi pathogen?
Fungi pathogens can be classified in various ways depending on their taxonomic classification, the type of infection they cause, and other factors. Here are some common ways to classify fungal pathogens:
Taxonomic classification: Fungal pathogens can be classified based on their taxonomic classification, such as Ascomycetes, Basidiomycetes, and Zygomycetes. For example, the fungus Aspergillus fumigatus belongs to the class Ascomycetes.
Systemic vs. superficial infections: Fungal pathogens can be classified based on the type of infection they cause, such as systemic or superficial infections. Systemic fungal infections involve fungi that spread throughout the body and can affect multiple organs, while superficial infections are limited to the skin, hair, and nails.
Opportunistic vs. primary pathogens: Fungal pathogens can also be classified based on their pathogenicity. Opportunistic pathogens are normally harmless fungi that can cause disease in people with weakened immune systems, while primary pathogens are fungi that can cause disease in healthy individuals.
Host specificity: Fungal pathogens can also be classified based on their host specificity. Some fungi are highly adapted to infect specific host species, while others can infect a wide range of hosts.
What is the life cycle of a fungi pathogen?
The life cycle of a fungal pathogen can vary depending on the specific species of fungus. However, most fungal pathogens have a life cycle that involves several distinct stages:
Spore formation: Fungal pathogens reproduce by producing spores, which can be dispersed by wind, water, or other means. Spores may be produced asexually or sexually, depending on the species.
Germination: When a spore lands on a suitable surface, it may germinate and produce a hypha, which is a thin, branching filament that can grow and spread.
Penetration: The hyphae of some fungal pathogens are capable of penetrating host tissues, such as the skin or mucous membranes, allowing the fungus to enter the host's body.
Invasion and colonization: Once inside the host's body, the fungus may continue to grow and spread, invading and colonizing tissues and organs. Fungal pathogens can cause a wide range of infections, from superficial infections of the skin and nails to deep-seated infections of the lungs, brain, or other organs.
Reproduction: In some cases, fungal pathogens may reproduce within the host's body, producing spores that can be released and spread to other hosts.
Survival and dissemination: Fungal pathogens may also have mechanisms for surviving within the host's body, such as producing protective structures called biofilms, which can help the fungus evade the host's immune system. Some fungal pathogens may also be capable of disseminating throughout the body, spreading from one organ to another, and causing widespread infection.
What are 5 examples of fungal plant pathogens?
Fungal plant pathogens are a diverse group of fungi that can cause a wide range of diseases in plants, including wilting, rotting, and leaf spots. Here are five examples of fungal plant pathogens:
Fusarium oxysporum: This fungus is a common cause of wilt disease in various plants, including tomatoes, melons, and bananas.
Botrytis cinerea: This fungus is a common cause of gray mold in many crops, including grapes, strawberries, and tomatoes.
Phytophthora infestans: This fungus-like pathogen is the cause of late blight in potatoes and tomatoes, a disease that was responsible for the Irish potato famine in the mid-1800s.
Rhizoctonia solani: This fungus is a common cause of root rot in many crops, including soybeans, sugar beets, and potatoes.
Colletotrichum spp: This group of fungi is responsible for anthracnose, a disease that can affect a wide range of plants, including mangoes, papayas, and avocadoes.
What are 3 harmful or pathogenic fungi?
There are many harmful or pathogenic fungi that can cause diseases in humans, animals, and plants. Here are three examples of such fungi:
Aspergillus fumigatus: This fungus is a common cause of aspergillosis, a serious lung infection that can be fatal in people with weakened immune systems. It can also cause allergies and other respiratory problems.
Candida albicans: This fungus is a normal part of the human microbiome but can become pathogenic and cause infections, especially in people with weakened immune systems. It can cause thrush, vaginal yeast infections, and invasive candidiasis, a serious bloodstream infection.
Puccinia graminis: This fungus is the cause of wheat rust, a disease that can devastate wheat crops and cause significant economic losses. It can also infect other cereal crops, such as barley and oats.







0 Comments